Mental Health and Exercise
By Nadia Butt [Get Well Clinic]
Defining mental illness and mental health
Mental illness is when the brain is not working the way it should, and as a result, it affects how a person behaves, thinks and feels. Mental illness often disrupts a person’s ability to function in society and interact with others (American Psychiatric Association, 2018). There is a collection of different types of mental illnesses such as depression, anxiety, bipolar disorder, schizophrenia and post-traumatic stress disorder. Individuals with mental illness may experience sadness, extreme feelings of worry, anger and/or mood changes (Lobo & Agius, 2012). However, since mental illnesses are on a spectrum, the severity of symptoms vary between individuals (Lobo & Agius, 2012).
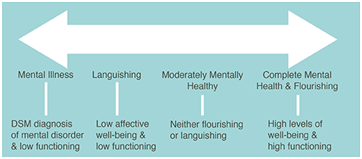
Figure 1. Mental Health Continuum Model (Every Moment Counts, n.d.)
Mental health is a state of well-being that everyone has. Good mental health often involves you having a sense of purpose, enjoying life and having the ability to cope with the stresses of life (World Health Organization, 2012). Even if you do not have a mental illness, throughout your life, you will experience strains from life events that affect your happiness and may cause stress, burnout, anxiety, or other negative feelings (Canadian Mental Health Association, 2020). Therefore, your mental health status changes throughout your life. Since mental health lies on a spectrum, you do not only experience the two extremes of good or bad mental health – there’s everything in between as well (Canadian Mental Health Association, n.d.). Additionally, if your mental health is significantly suffering or you are experiencing poor mental health for a significant amount of time, you can eventually acquire a mental illness (Franken et al., 2018). This can be explained through the mental health continuum model (refer to figure 1), which consists of having mental health and mental illness at two endpoints (Franken et al., 2018). In this model, an individual can lie at one point of the continuum and later on move positions depending on if their mental health improves or deteriorates (Franken et al., 2018).
It is important to note that mental health is not just a lack of mental illness – you can have bad mental health without a mental illness (Westerhof & Keyes, 2010). Similarly, if you have a mental illness, it does not mean you cannot achieve good mental health (Westerhof & Keyes, 2010). Someone with mental illness can live a healthy life. Moreover, it is important to remember that mental health concerns are health problems, just like arthritis and diabetes. Thus, mental health problems are just as concerning as physical health problems.
Introduction
Every year, one in five people living in Canada will be affected by a mental illness (Mental Health Commission of Canada, 2013). By the age of 40, one in two people will be affected by a mental illness (Mental Health Commission of Canada, 2013). Mental illness is so prominent in our population because no one is immune to it. COVID-19 has only made matters worse, as many more Canadians are facing serious mental health problems, which can lead to more people experiencing mental illnesses. An astounding 50% of Canadians feel that their mental health is worsening throughout the pandemic (Angus Reid Institute, 2020). So, what is something you can do to help improve your mental health? Exercise.
Regardless of mental health status, you should exercise
We all know that exercise is beneficial. You hear it all the time. That you should exercise because it’s “good for you.” But can exercise really help you? Well, a large-scale study which consisted of 1.2 million people found that exercise significantly helps to improve mental health. The study found a 43.2% reduction in the number of poor mental health days experienced by individuals who exercise regularly than those who do not exercise (Chekroud et al., 2018). Therefore, if you are doing “okay,” exercise can help improve your mental health. Likewise, if you are doing “good” you should still exercise, as exercise can prevent future mental health problems. This is because happy” hormones are created and released in our brain during exercise, such as endorphins. Endorphins help us feel good and alleviate pain and stress (Orlova et al., 2008). Additionally, dopamine, norepinephrine, and serotonin are other “happy” hormones released in the brain during exercise; they play an important role in regulating mood (Lin & Kuo, 2013). Contrastingly, exercise not only increases “happy” hormones but also reduces stress hormones, such as cortisol (Exercising to Relax, 2020). In fact, mental health medications often work by regulating the activity of these hormones in the brain (Dfarhud et al., 2014; Dremencov et al., 2009). Thus, regardless of your mental health status, you should exercise as it helps you achieve and preserve good mental health.
Exercise not only helps mental health but can also help prevent the development of mental illnesses. For instance, individuals who exercise are 17% less likely to develop depression (Schuch et al., 2018). Exercise even reduces the likelihood of depression for individuals with high genetic risk for this disease (Choi et al., 2019). Similarly, another study found that rigorous exercise protects individuals from certain anxiety disorders and post-traumatic stress disorders (Schuch et al., 2019). To further explore the benefits of exercise on mental illness, three mental health disorders – anxiety, PTSD and depression – will be discussed.
Exercise helps those who have mental illnesses
Anxiety
Exercise has been proven to help those who have anxiety by being a form of exposure therapy (DeBoer et al., 2012). This is because anxiety disorders and moderate-intensity exercises share similar symptoms (Broman-Fulks & Storey, 2008). Your body tenses, you sweat, your heart races and your respiratory rate increases when you feel anxious and when you exercise. Therefore, exercising can expose individuals to anxiety symptoms in a manner that is safe, which allows individuals to become less sensitive to these symptoms (DeBoer et al., 2012). This is because individuals learn to link these symptoms with feelings of excitement and enjoyment, rather than danger. Consequently, individuals with anxiety and who exercise are less likely to panic when experiencing these linked symptoms, helping them recover from anxiety disorders (DeBoer et al., 2012).
Post-traumatic stress disorder
Exercise helps individuals who suffer from post-traumatic stress disorder (PTSD). A study revealed that individuals who exercise experience fewer PTSD symptoms than those who do not exercise (Fetzner & Asmundson, 2015). Specifically, studies have shown that individuals who undergo exposure therapy–a popular treatment option–and exercise have higher levels of brain-derived neurotrophic factor (BDNF) than those who only participate in exposure therapy (Powers et al., 2015). BDNF is a protein that is important to reduce conditioned fear experienced by those with trauma (Powers et al., 2015). Thus, it is best for individuals recovering from PTSD to combine exercise with other treatment options. Moreover, individuals with PTSD greatly benefit from focusing on their body and how they feel while exercising. This mindfulness helps their nervous system become “unstuck,” allowing their body to depart out of the immobilization stress response caused by PTSD (Smith et al., 2020; Williamson et al., 2015).
Depression
Exercise is found to reduce depressive symptoms and, in some cases, can be just as beneficial as antidepressants and psychotherapies (Blumenthal et al., 2012). Interestingly, a study found that depressed individuals who exercise regularly are less likely to have depressive symptoms in the long-term than those who are taking antidepressants (Craft & Perna, 2004). So how does exercise helps to combat depression? One reason is that exercise helps the growth of new neurons by increasing the release of proteins called neurotrophic factors (Gujral et al., 2017). Consequently, this neuronal growth increases neuron connections, particularly in the region of the brain called the hippocampus (Gujral et al., 2017). The hippocampus is responsible for regulating mood, and as a result, the increased activity of neurons in this brain region helps relieve depression (Gujral et al., 2017). Evidently, individuals who are depressed experience hippocampal atrophy, and consequently have abnormally small hippocampi (Gujral et al., 2017). Thus, exercise prevents brain atrophy and can increase the hippocampus size through neuronal growth (Gujral et al., 2017).
What should you do?
Studies have shown that aerobic exercise is the best type of exercise to help manage mental illnesses and improve mental health (Chekroud et al., 2018). Aerobic exercise includes running, biking, hiking, jumping rope, swimming and dancing. Also, group activities like fitness classes and team sports can improve your mental health by providing you with opportunities for social interactions (Chekroud et al., 2018). During the pandemic, you should consider exercising with others virtually. Furthermore, the Canadian Physical Activity Guidelines and the Canadian Society for Exercise Professionals recommends that adults between the age of 18-64 should exercise 30-60 minutes a day for a total of 150 minutes of exercise a week.
If you or a loved one is struggling with mental health, here are some resources available to you
- Get Well Clinic has a mental health program that integrates medical assessments, medications, psychotherapy and counselling to help you get better. You can contact our mental health coordinator or ask your family doctor to refer you.
- 211 Ontario: Call 211 or the toll-free number at 1-877-330-3213 to receive information about mental health resources available to you.
- BounceBack: Call the toll-free number at 1-866-345-0224 to participate in a free cognitive behavioural therapy (CBT) based program to support your mental health. The program is available for individuals who are at least 15 years old.
- Good2Talk: Call the toll-free number at 1-866-925-5454 or text good2talkon to 686868 if you’re aged 17 to 25 and need someone to talk to.
References:
American Psychiatric Association. (2018, August). What Is Mental Illness? https://www.psychiatry.org/patients-families/what-is-mental-illness.
Angus Reid Institute. (2020). Worry, gratitude & boredom: As Covid-19 affects mental, financial health, who fares better; who is worse? http://angusreid.org/covid19-mental-health/avenue for the treatment of anxiety disorders. Expert review of neurotherapeutics, 12(8), 1011–11022. https://doi.org/10.1586/ern.12.73
Blumenthal, J. A., Smith, P. J., & Hoffman, B. M. (2012). Opinion And Evidence. ACSM's Health & Fitness Journal,16(4), 14-21.https://doi.org/10.1249/01.fit.0000416000.09526.eb
Broman-Fulks, J. J., & Storey, K. M. (2008). Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety, Stress & Coping, 21(2), 117-128. https://doi.org/10.1080/10615800701762675
Canadian Mental Health Association. (2020, January 13). Mental health: What is it, really? CMHA National. https://cmha.ca/blogs/mental-health-what-is-it-really.
Canadian Mental Health Association. (n.d.). What's the difference between mental health and mental illness? What's the difference between mental health and mental illness? | Here to Help. https://www.heretohelp.bc.ca/q-and-a/whats-the-difference-between-mental-health-and-mental-illness.
Chekroud, S. R., Gueorguieva, R., Zheutlin, A. B., Paulus, M., Krumholz, H. M., Krystal, J. H., & Chekroud, A. M. (2018). Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. The Lancet Psychiatry, 5(9), 739–746. https://doi.org/10.1016/s2215-0366(18)30227-x
Choi, K. W., Zheutlin, A. B., Karlson, R. A., Wang, M. J., Dunn, E. C., Stein, M. B., … Smoller, J. W. (2019). Physical activity offsets genetic risk for incident depression assessed via electronic health records in a biobank cohort study. Depression and Anxiety, 37(2), 106–114. https://doi.org/10.1002/da.22967
Craft, L. L., & Perna, F. M. (2004). The Benefits of Exercise for the Clinically Depressed. The Primary Care Companion to The Journal of Clinical Psychiatry, 06(03), 104-111. https://doi.org/10.4088/pcc.v06n0301
DeBoer, L. B., Powers, M. B., Utschig, A. C., Otto, M. W., & Smits, J. A. (2012). Exploring exercise as an avenue for the treatment of anxiety disorders. Expert Rev Neurother. 2012 Aug;12(8):1011-22. doi: 10.1586/ern.12.73. PMID: 23002943; PMCID: PMC3501262.
Dfarhud, D., Malmir, M., & Khanahmadi, M. (2014). Happiness & Health: The Biological Factors-Diamond, A., McIntyre, C., & Smits, J. A. (2015). Exercise Augmentation of Exposure Therapy for PTSD: Rationale and Pilot Efficacy Data. Cognitive behaviour therapy, 44(4), 314–327. https://doi.org/10.1080/16506073.2015.1012740
Dremencov, E., Mansari, M., & Blier, P. (2009). Brain Norepinephrine System as a Target for Antidepressant and Mood Stabilizing Medications. Current Drug Targets, 10(11), 1061-1068. https://doi.org/10.2174/138945009789735165
Every Moment Counts. (n.d.). Mental Health Continuum [Figure]. https://everymomentcounts.org/view.php?nav_id=33
Exercising to relax. (2020, July 7). https://www.health.harvard.edu/staying-healthy/exercising-to-relax
Fetzner, M. G., & Asmundson, G. J. (2015). Aerobic Exercise Reduces Symptoms of in PTSD accelerates physiological aging. Frontiers in psychology, 5, 1571. https://doi.org/10.3389/fpsyg.2014.01571
Franken, K., Lamers, S., Ten Klooster, P. M., Bohlmeijer, E. T., & Westerhof, G. J. (2018). Validation of the Mental Health Continuum-Short Form and the dual continua model of well-being and psychopathology in an adult mental health setting. Journal of clinical psychology, 74(12), 2187–2202. https://doi.org/10.1002/jclp.22659
Gujral, S., Aizenstein, H., Reynolds, C. F., 3rd, Butters, M. A., & Erickson, K. I. (2017). Exercise effects on depression: Possible neural mechanisms. General hospital psychiatry, 49, 2–10. https://doi.org/10.1016/j.genhosppsych.2017.04.012
Lin, T., & Kuo, Y. (2013). Exercise Benefits Brain Function: The Monoamine Connection. Brain Sciences, 3(4), 39-53. https://doi.org/10.3390/brainsci3010039
Lobo, D. M., & Agius, M. (2012). The mental illness spectrum. Psychiatria Danubina, 24 Suppl 1, S157–S160.
Mental Health Commission of Canada. (2013). Making the Case for Investing in Mental Health in Canada. https://www.mentalhealthcommission.ca/sites/default/files/2016-06/Investing_in_Mental_Health_FINAL_Version_ENG.pdf.
Powers, M. B., Medina, J. L., Burns, S., Kauffman, B. Y., Monfils, M., Asmundson, G. J., Posttraumatic
Stress Disorder: A Randomized Controlled Trial. Cognitive behaviour therapy, 44(4), 301–313. https://doi.org/10.1080/16506073.2014.916745
Schuch, F. B., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P. B., Silva, E. S., Hallgren, M., Ponce De
Leon, A., Dunn, A. L., Deslandes, A. C., Fleck, M. P., Carvalho, A. F., & Stubbs, B. (2018). Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. The American journal of psychiatry, 175(7), 631–648. https://doi.org/10.1176/appi.ajp.2018.17111194
Schuch, F. B., Stubbs, B., Meyer, J., Heissel, A., Zech, P., Vancampfort, D., … Hiles, S. A. (2019). Physical activity protects from incident anxiety: A meta‐analysis of prospective cohort studies. Depression and Anxiety, 36(9), 846–858. https://doi.org/10.1002/da.22915
Smith, M., Robinson, L., Segal, R., & Segal, J. (2020, November). Post-Traumatic Stress Disorder (PTSD). https://www.helpguide.org/articles/ptsd-trauma/ptsd-symptoms-self-help-treatment.htm.
Tendzegolskis, Z., Viru, A., & Orlova, E. (2008, March 14). Exercise-Induced Changes of Endorphin Contents in Hypothalamus, Hypophysis, Adrenals and Blood Plasma. https://www.thiemeconnect.de/products/ejournals/abstract/10.1055/s-2007-1024721
Westerhof, G. J., & Keyes, C. L. (2010). Mental Illness and Mental Health: The Two Continua Model Across the Lifespan. Journal of adult development, 17(2), 110–119. https://doi.org/10.1007/s10804-009-9082-y
Williamson, J. B., Porges, E. C., Lamb, D. G., & Porges, S. W. (2015). Maladaptive autonomic regulation in PTSD accelerates physiological aging. Frontiers in psychology, 5, 1571. https://doi.org/10.3389/fpsyg.2014.01571
World Health Organization. (2012, May 11). WHO urges more investments, services for mental health. World Health Organization. https://www.who.int/mental_health/who_urges_investment/en/.












